*It has been reported that the total volume of HGPIN increases with increasing pathologic stage with a significant correlation between volume of HGPIN and the number of lymph node metastases.(1)
*HGPIN by itself does not appear to elevate serum PSA levels.(1)
*The distinction between low and high grade PIN is based on the degree of architectural complexity and more importantly, on the extent of cytologic abnormalities. In low grade PIN, there is proliferation and "piling
up" of secretory cells of the lining epithelium with irregular spacing. Some nuclei have small, usually inconspicuous nucleoli while a few may contain more prominent nucleoli. (1)
*High grade PIN is characterized by a more uniform morphologic alteration.Cytologically, the acini and ducts are lined by malignant cells with a variety of architectural complexity and patterns.The individual cells are almost uniformly enlarged with increased nuclear/cytoplasmic ratio, therefore showing less variation in nuclear size than that seen in low grade PIN. Many cells of HGPIN contain prominent nucleoli and most show coarse clumping of the chromatin that is often present along the nuclear membrane.(1)
*Four patterns of HGPIN have been described, which are ;
- flat: atypia without significant architectural changes
- tufting: nuclei become
more piled up, resulting in undulating
mounds of cells
- micropapillary: columns of atypical epithelium that typically
lack fibrovascular cores
- cribrifrom: more complex architectural
patterns appear such as Roman
bridge and cribriform formation (1)
*Despite alL this Evidence , we dont know the natural history of PIN, and in particular how often it progresses to cancer. Thus,unlıke in cancer of the cervix, the term "Carcinoma in situ" is not used for PIN.
for slides ; http://www.surgicalpathologyatlas.com/glfusion/mediagallery/media.php?f=0&sort=0&s=20080802171141419
(1) WHO- Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs
22 Mayıs 2012 Salı
19 Mayıs 2012 Cumartesi
Inflammatory Conditions III
Postbiopsy Granlomas:
- After 9 days to 52 months of transurethral resection.
- Although its much more common to have granulomatous rxn following TUR similar linear granulomas may rarely develop following a needle bx.
- Postbiopsy granulomas are composed of central region of fibrinoid necrosis surrounded by palisading epithelioid histiocytes.
- In contrast to infectious granulomas, the necrosis in postbiopsy granulomas often contains ghost lıke structures of vessels, acini and stroma.
- Wedge shaped granulomas , irregularity of their shapes (granulomas) distinguishes these granulomas from infectious granulomas.
- Postbiopsy granulomasalso rarelyoccur following a needle bx.
- The postbiopsy granulomas appears to be a rxn to altered epithelium and stroma from the trauma of previous cautery.
- Posrbiopsy granulomas are asymptomatic, incidental findings requiring no treatment.
- Cases with eosinophilia such as allergic granulomatous prostatitis - Church Strauss ,without eosinophlia- Wegener
- Histopathology; multiple, small , ovoid, granulomas surrounded by numerous eosinophils.
- Regularity of size and shape of these granulomas, the eosinophilic necrosis within the granulomas and extensive infiltration of eosinophils throughout stroma, not just surrounding the granulomas , seperate this entitiy from that of postbiopsy ranulomas with eosinophils.
Inflammatory Conditions II
Granulomatous Prostatitis:
*infectious granulomas
*nonspesific granulomatous prostatitis
*postbiopsy resection granulomas
*systemic granulomatous prostatitis
Mycotic Prostatitis:
*Source: Biopsy Interpretation of the Prostate -Jonathan I. Epstein
*infectious granulomas
*nonspesific granulomatous prostatitis
*postbiopsy resection granulomas
*systemic granulomatous prostatitis
Mycotic Prostatitis:
- Immuncompromised hosts
- Blastomycosis, coccidiomycosis, cryptococcosis (most common)
- Can be seen in systemic tbc but nowadays its commonly seen in as a complication of BCG immunotherapy for superficialbladder carcionoma.
- Hitologically the findings in BCG prostatitis are indistinguishable from those of tbc prostatitis occuring as a result of systemic infection.
- In 25387 benign specimens of the %5
- In the etiologyof this lession is thought to be rxn to bacterial toxins, cell debris, and secretions spilling into the stroma fro blocked ducts.
- Mimics prostate carcinoma on rectal examination and USG.
- Earliest lesions; dilated ducts and acini filled with neutrophils, debris, foamy histiocytes and desquamated epithelial cells. Rupture of these ducts and acini results in a localized gralunomatous and chronic inflammatory rxn. Older lesions of nonspesific granulomatous prostatitis show a more prominent fibrous component.
- Treated with warm sitz baths, fluids and antibiotics.
- Although small abscesses may be present at the center of nodules of nonspesific granulomatous prostatitis, caseous necrosis is absent.
*Source: Biopsy Interpretation of the Prostate -Jonathan I. Epstein
Inflammatory Conditions I
Acute and Chronic Prostatic Inflammation:
*Source: Biopsy Interpretation of the Prostate -Jonathan I. Epstein
- Diagnosed clinically and treated by antibiotics.
- Acute prostatitis ; - sheets of neutrophils within the acini -intraductal desquamated cellular debris - stromal edema ad hyperemia
- The biopsy of TUR of a man with clinical acute prostatitis is contraindicated, can result in sepsis or other complications such as stricture.
- Should be diagnosed as "prostate tissue with acute inflammation"
- Prostatic abscesses ; bladder outlet obstruction secondary to a lower urinary tract infection, usually due to coliform organisms. Much less frequently dissemination from skin -stafilococcus or complication of biopsy or instrumentation.
- Chronic inflammation (in BPH) and chronic prostatitis distinguish is difficult
- Prostatitis may lead to serum PSA elevation.
- We comment on the histologic presence of chronic inflamation only when its prominent.
- As in bladder majority of man prostatic malokoplakia have urinary infection , most frequently with E.coli.
- In USG prostatic induration and hipoechoic lesion.
- Michaelis Gutmann bodies
*Source: Biopsy Interpretation of the Prostate -Jonathan I. Epstein
9 Mayıs 2012 Çarşamba
Benign Prostatic Hyperplasia
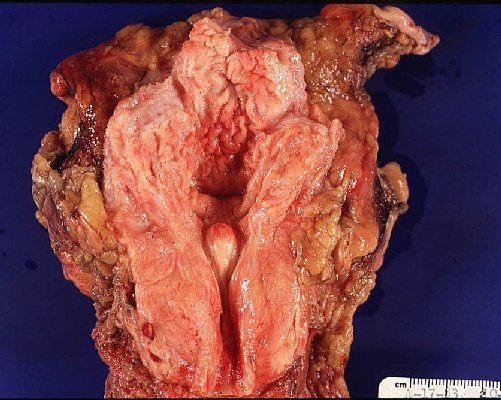 *Paraurethral component of the prostate gland undergo nodular glandular hyperplasia accompanied y the hyperplasia of the intervening fibromuscular stroma of the gland.The periphera glandular components of the prostate are not involved in this process and become compressed and atrophic at the outer margin.(1)
*Paraurethral component of the prostate gland undergo nodular glandular hyperplasia accompanied y the hyperplasia of the intervening fibromuscular stroma of the gland.The periphera glandular components of the prostate are not involved in this process and become compressed and atrophic at the outer margin.(1)*BPH ; has a nodular microcystic appareance, tiny cysts epresenting dilated hyperplastic prostatic asini.(1)
*The earliest BPH nodules are predominantly stromal and are composed mainly of fibrous tissue admixed with some smooth muscle and more numerous BPH nodules are typically more situated within the transition zone. (2)
 |
| http://www.cap.org/apps/docs/reference/myBiopsy/prostate_benign.html |
*Benign needle biopsy specimens of the prostate should be diagnosed as “benign prostate tissue,” not as “benign prostatic hyperplasia.” First, many needle biopsy specimens do not even sample the transition zone. Second, histologic findings on needle biopsy, with the exception of stromal nodules, do not correlate with size of the prostate or urinary obstructive symptoms . Finally, signing out a specimen as “BPH” may falsely reassure the urologist that a palpable or hypoechoic lesion of concern has been sampled.(2)
*Within areas of BPH, nodules or a diffuse stromal infiltrate of
lymphocytes and plasma cells are commonly seen in a peri-glandular distribution.
However, in the majority of cases these findings have not been identified with
an infectious process or clinical symptoms of prostatitis. (2)
*Prostatic infarcts can be found in approximately 20% to 25% of specimens removed for BPH and immediately adjacent to the infarcts, reactive epithelial nests with prominent nucleoli, some pleomorphism, and even atypical mitotic figures can be seen, mimicking urothelial or squamous cell carcinoma. Progressing away from the center of the infarct, more mature squamous metaplasia is seen. (2)
*(1) Functional Histology-A Text And the Colour Atlas - P.R.Wheather
*(2) Sternberg's Diagnostic Surgical Pathology, 5th Edition
Histology Of The Prostate
*Prostate glands consists of glandular lobules, up to 50 in al, which converge to open via about 20 seperate ducts into irregular outpockets of the prostatic urethra.(1)
*Ejeculatory ducts join the prostatic urethra just before its exit from the prostate gland.(1)
*Secretory product of the postate, which makes up about 75% of the seminal fluid.(1)
*The prostataic glandular epithelıum varies from inactive, low cuboidal to active, pseudostratified columnar depending on the degre of stimulation by androgen.(1)
*The secrotory product is stored temporarily within the gland and often forms amorphous masses called corpora amylacea.(1)
*Utricule is the Müllerian remnant.
* The peripheral zone contains the main glands located posterio-laterally in the outer parenchyma of the gland and is the site most susceptible to inflammation (prostatitis) and malignant neoplasia.(2)
*The central zone is the region surrounding the utricle and ejaculatory ducts. Interestingly, this zone is relatively resistant to inflammation and hyperplasia. (2) It may look like H-PIN.
*The transitional and periurethral zones surrounds the prostatic urethra and contains submucosal and mucosal glands that undergo non-cancerous proliferation, leading to benign prostatic hypertrophy (BPH). (2) McNeal's model of zonal anatomy of the prostate
for virtual microscopy :
http://141.214.65.171/Histology/Male%20Reproductive%20System/281_HISTO_40X.svs/view.apml
*(1)Functional Histology-A Text And the Colour Atlas - P.R.Wheather
*(2)http://histology.med.umich.edu/medical/male-reproductive-system
*Ejeculatory ducts join the prostatic urethra just before its exit from the prostate gland.(1)
*Secretory product of the postate, which makes up about 75% of the seminal fluid.(1)
*The prostataic glandular epithelıum varies from inactive, low cuboidal to active, pseudostratified columnar depending on the degre of stimulation by androgen.(1)
*The secrotory product is stored temporarily within the gland and often forms amorphous masses called corpora amylacea.(1)
*Utricule is the Müllerian remnant.
* The peripheral zone contains the main glands located posterio-laterally in the outer parenchyma of the gland and is the site most susceptible to inflammation (prostatitis) and malignant neoplasia.(2)
*The central zone is the region surrounding the utricle and ejaculatory ducts. Interestingly, this zone is relatively resistant to inflammation and hyperplasia. (2) It may look like H-PIN.
*The transitional and periurethral zones surrounds the prostatic urethra and contains submucosal and mucosal glands that undergo non-cancerous proliferation, leading to benign prostatic hypertrophy (BPH). (2) McNeal's model of zonal anatomy of the prostate
for virtual microscopy :
http://141.214.65.171/Histology/Male%20Reproductive%20System/281_HISTO_40X.svs/view.apml
*(1)Functional Histology-A Text And the Colour Atlas - P.R.Wheather
*(2)http://histology.med.umich.edu/medical/male-reproductive-system
24 Temmuz 2011 Pazar
Pheochromocytoma
- Pheochromocytomas have been associated with "rule of 10s". 10% extraadrenal, bilateral, biologically malign, are not associatd with hypertension.
- Malignancy is more common ( 20-40%) in extra adrenal paragangliomas.
- The incidence of malinancy is higher ( 30%) in tumors that arise on the backdrop of germline SDHB mutations. The succinate dehydrogenase complex subunit gense ( SDHB, SDHC and SDHD) encode proteins involved in mitochondrial electron transport and oxygen sensing. The loss of funtion in one or more of these subunit leads to stabilization of the oncogenic transcription factor hypoxia-inducible factor 1a (HIF-1alfa), promoting tumorigenesis.
- Incubation of fresh tissue with a potassium dichromate solutıon turns the tumor a dark brown color due to oxidation of stored catecholamines, thus the term chromaffin.
- The histologic patern in pheochromocytoma is quite variable. Tumors are composed of polygonal to spindle-shaped chromaffin cellls or chief cells, clustered with sustentecular cells into small nests or alveoli(zellballen) by rich vascular network.
- Determinig malignancy in pheo, there is no histologic feature that reliably predicts clinical behaviour. The definitive diagnosis in pheo is based exclusively on the presence of metastases.
- Laboratory diagnosis is based on the increased urinary excreation of free catecholamines and their metabolites, such as vanillylmandelic acid and metanephrines.
- Tradement surgical excision + adrenergic blocking agents (for hypertensıon crisis).
- for histopathology video ; http://www.youtube.com/watch?v=7yjxG3KmX98
Kaydol:
Kayıtlar (Atom)




